70M WITH SEPTIC SHOCK 2 TO UROSEPSIS WITH B/L RENAL CALCULUS WITH B/L HYDOROURETERONEPHROSIS
GEN MEDICINE
This is an online e log book to discuss our patient de-identified health data shared after taking his/her/guardians signed informed consent.
Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evidence based input
This E blog also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box is welcome
I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
CHEIF COMPLAINTS:
Patient came with cheif complaints of abdominal pain in Right lower quadrant of abdomen since 1week
HISTORY OF PRESENT ILLNESS:
Patient was apparently asymptomatic 1week back then he developed pain in the Right lower quadrant abdomen which is
spasmodic type , intermittent, non radiating
H/o fever present which is intermittant, relieved on medication
H/o vomittings present(immediately after intake of food) which is non bilious non-projectile With food as content
PAST HISTORY:
Daily routine:
he used to Woke up at 5am, had breakfast around 7am he used to roam in street He packed his lunch which he ate at his workplace around 1pm, and came home by 4pm
He ate at 8pm and slept at 10pm.
50 years back he had a pelvic surgery (transurethral cystolitholapaxy) for removal of bladder stone
* There is no history of similar complaints in the past.
* he is not a known case of Diabetes, Hypertension, Asthama, Epilepsy, Tuberculosis.
Personal history:-
Diet - mixed
Appetite- normal
Sleep - adequate
Bowel and bladder movements - regular.
Alcohol consumption since 20 yrs and currently consumes 45 ml of alcohol daily.
GENERAL EXAMINATION
On examination, patient is conscious, coherent and cooperative and he is well oriented to time place and person
He is moderately built and well nourished
*Pallor - absent
*Icterus- present
*Clubbing-absent
*Cyanosis-absent
*Lymphadenopathy-absent
* Edema- absent
Vitals:-
BP- 120/70 mmHg
RR- 20cpm
PR-111bPm
Spo2- 99%at RA.
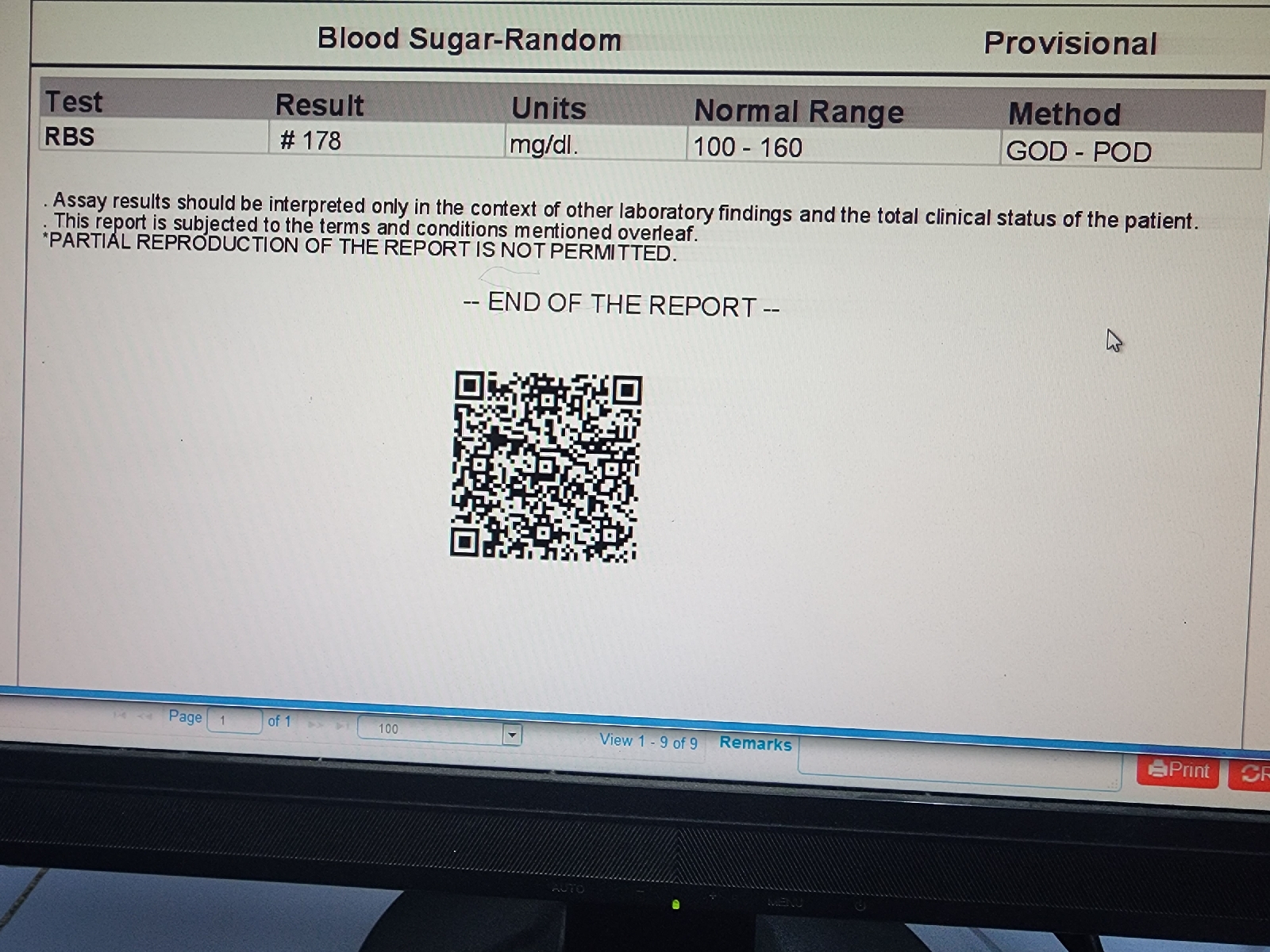
GRBS- 126mg/dl
SYSTEMIC EXAMINATION:
CVS: S1 and S2 heard. No addded thrills or murmurs heard
RESPIRATORY SYSTEM:
Normal vesicular breath sounds heard.
ABDOMEN:
*non tender
*soft
CNS:
Conscious and coherent.
Normal sensory and motor responses
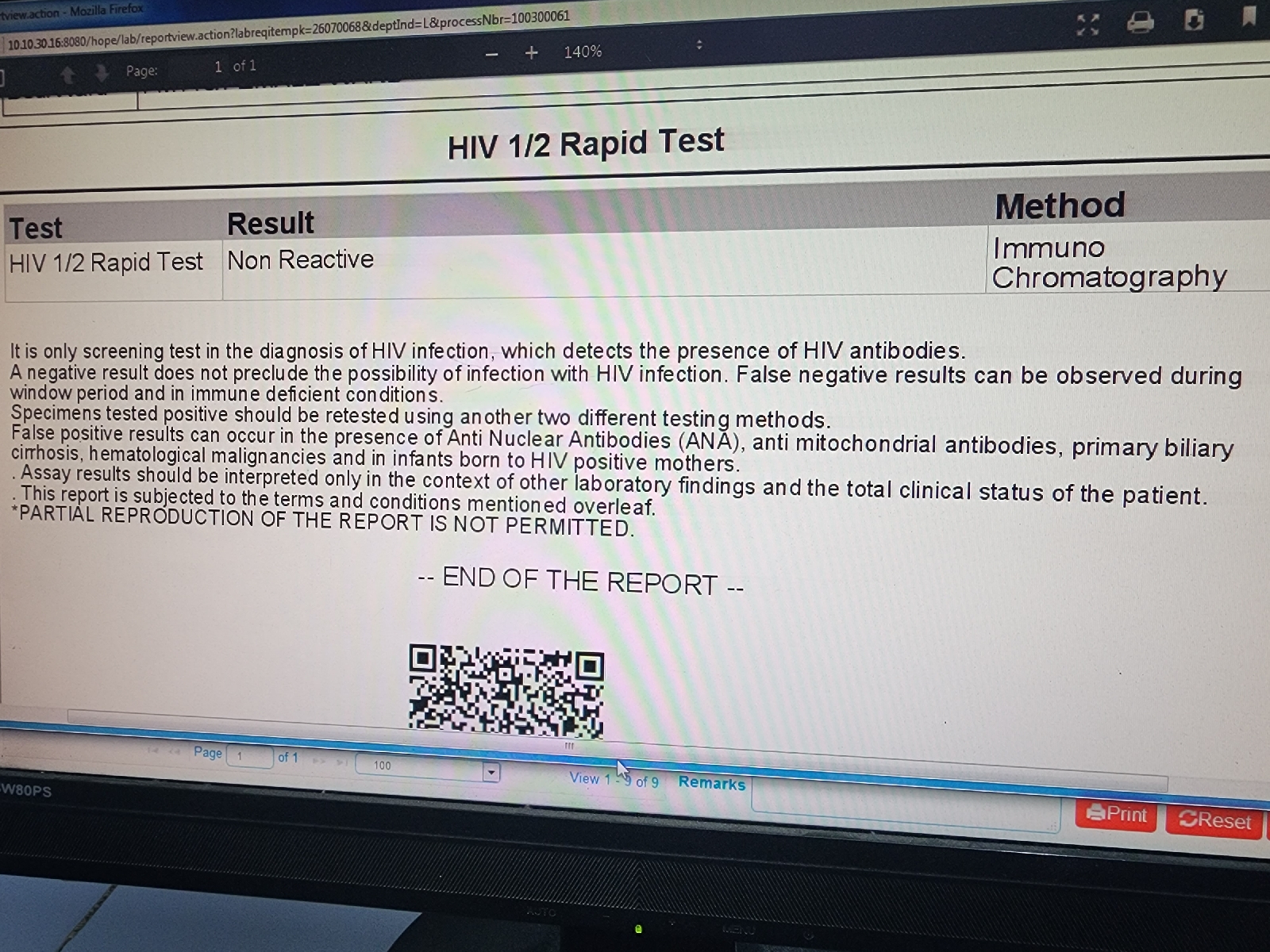
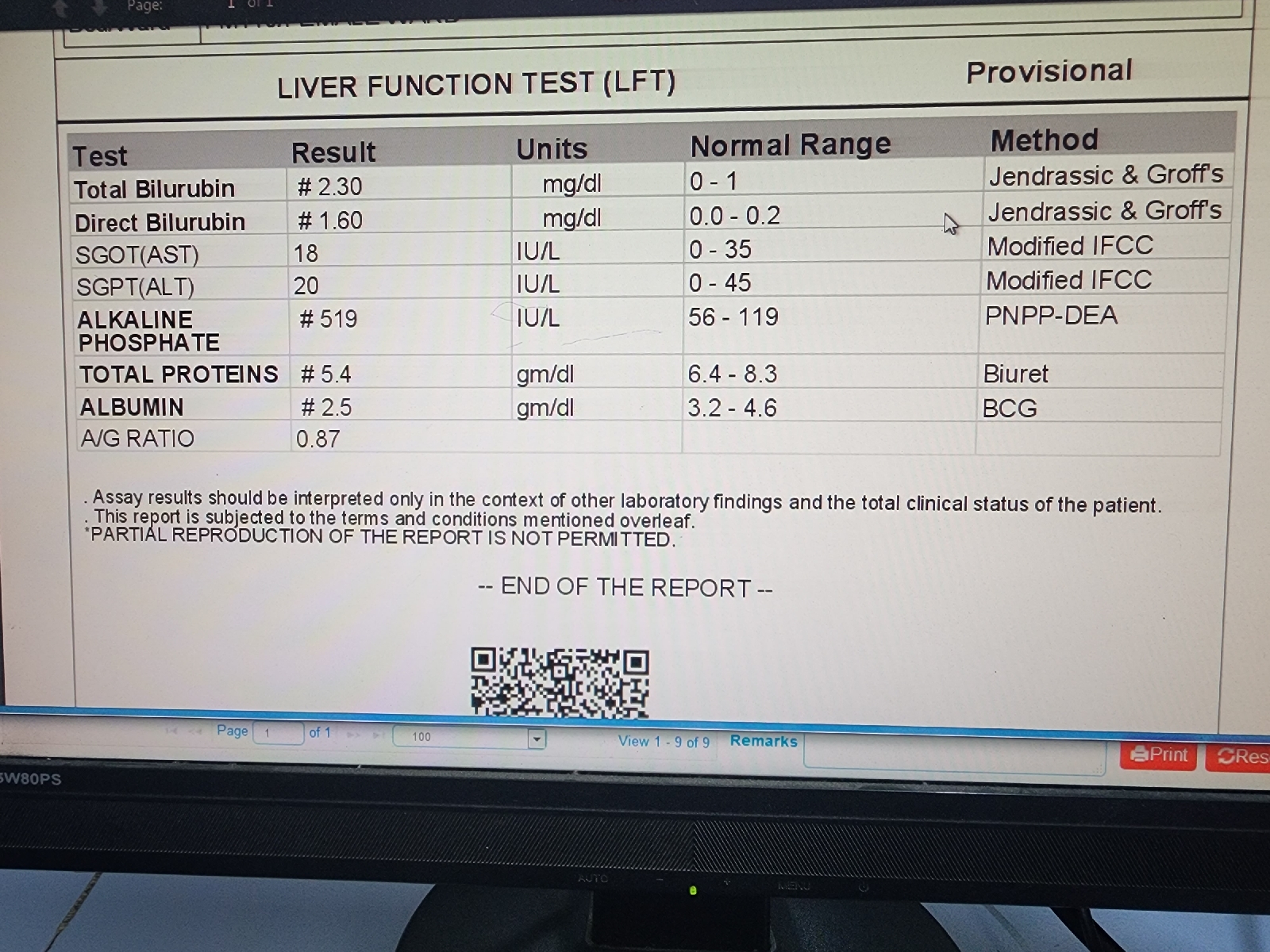
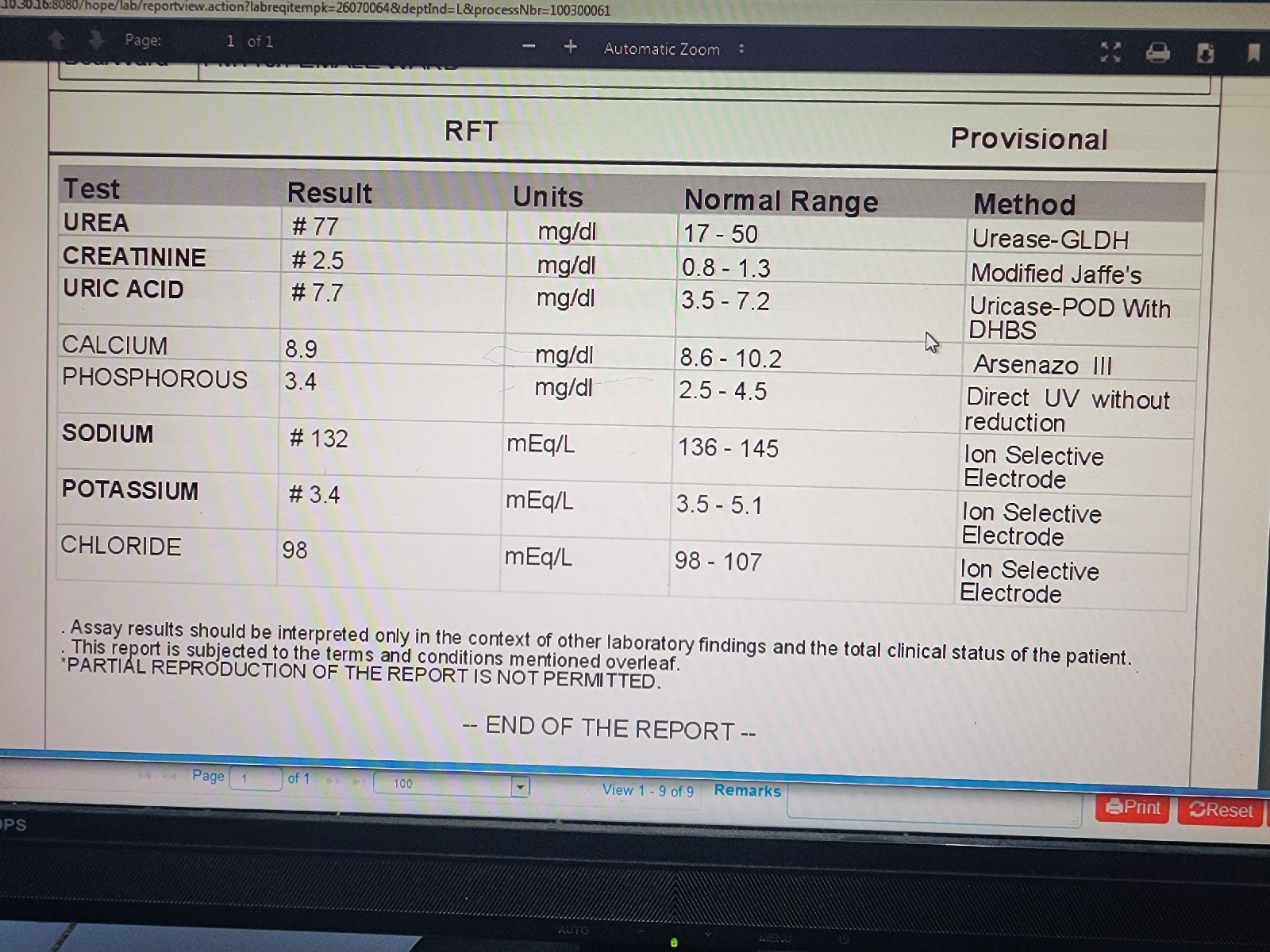
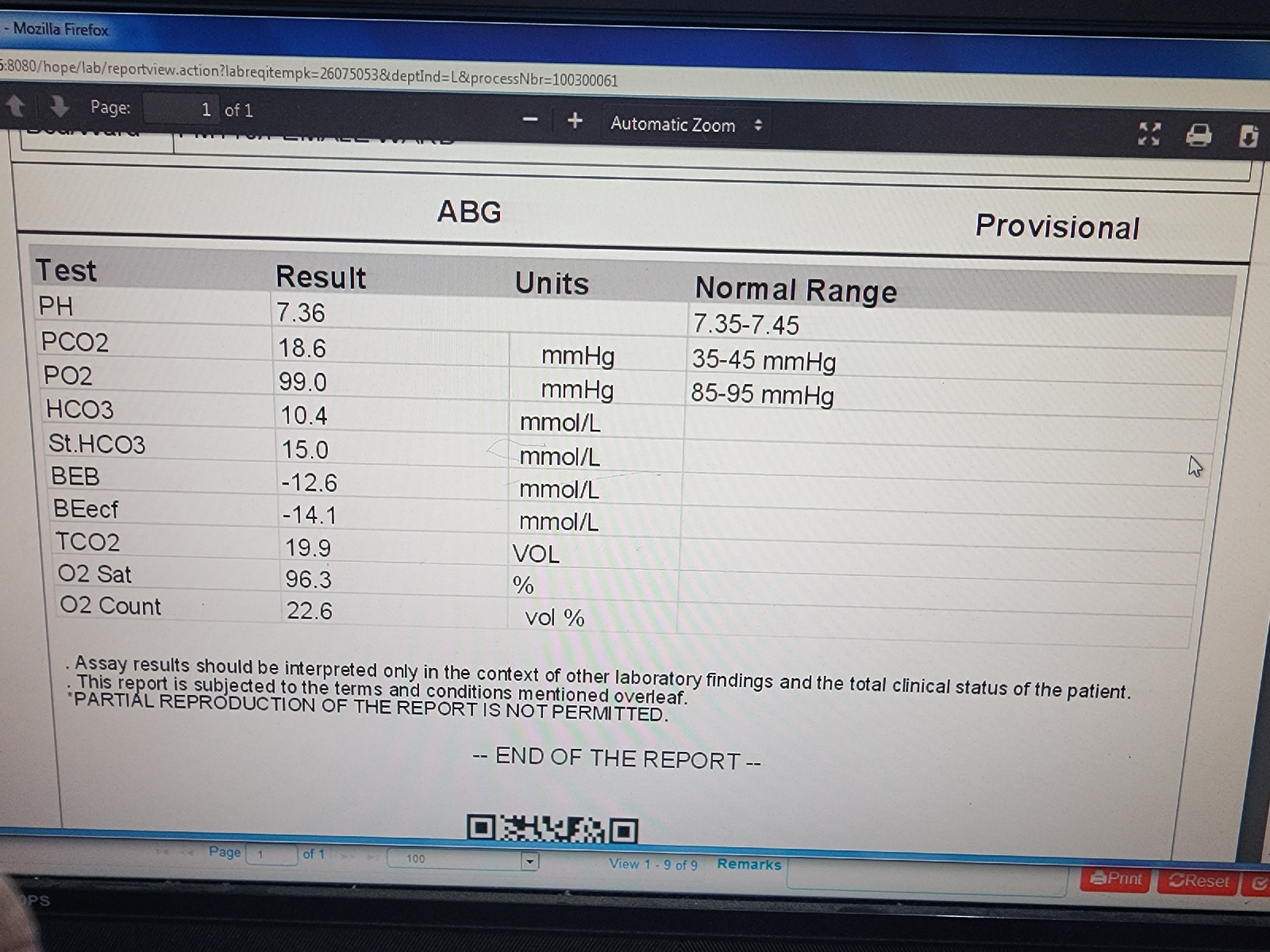
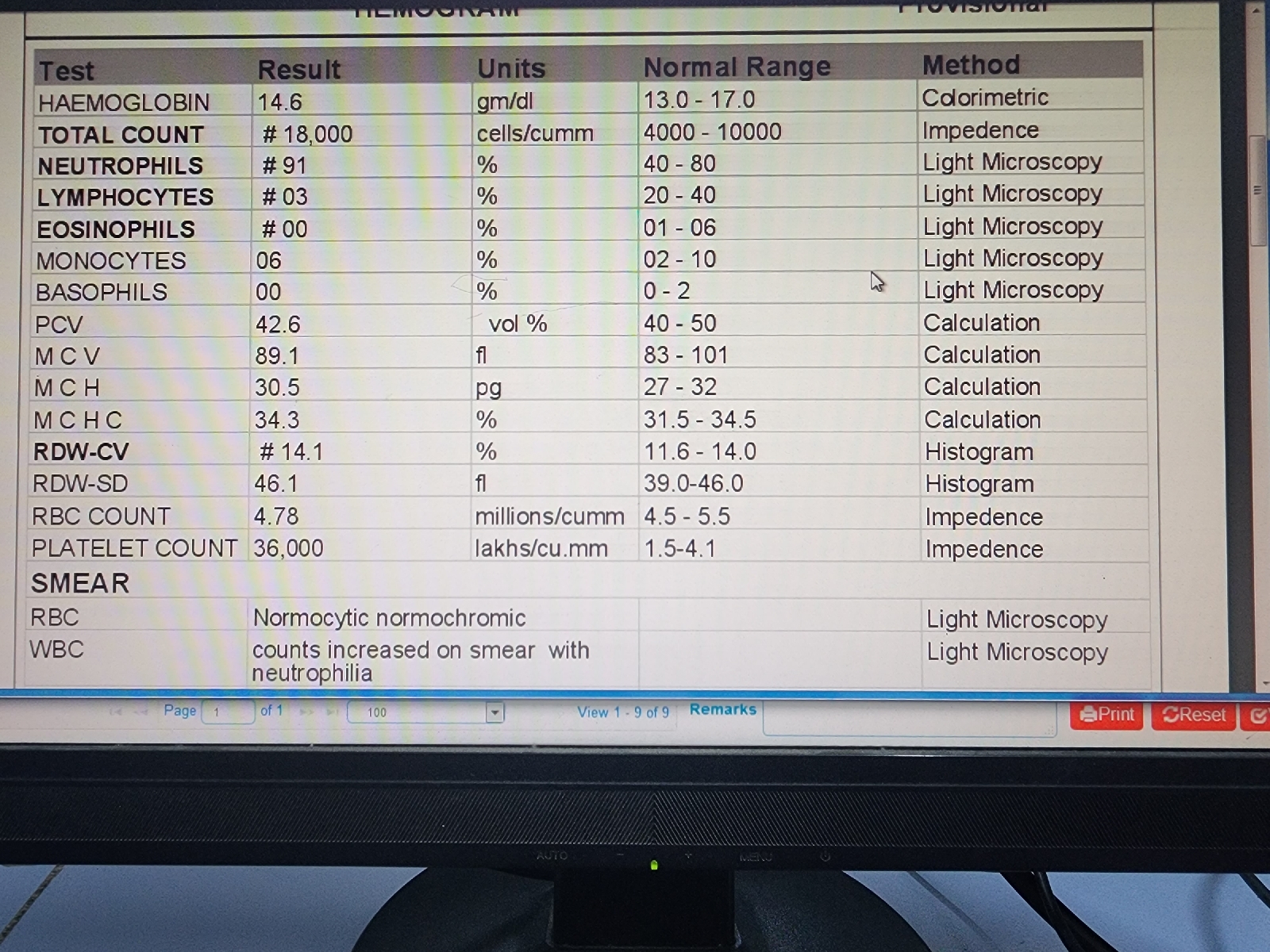
INVESTIGATIONS :
(8-08-23)
9-09-23
10-08-23
PROVISIONAL DIAGNOSIS:
SEPTIC SHOCK 2 TO UROSEPSIS WITH B/L RENAL CALCULUS WITH B/L HYDOROURETERONEPHROSIS
TREATMENT:
1) Iv Fluias 20ns @75ml/hr
2) inj norad 46ml Ns +4ml
3) inj buscopan im/OD
4) inj pipal 2.25 iv/tid
5) inj metronidazole 500mg iv tid
6) inj vasopressin 2ml +38ml ns @ 0.6ml /hr
8)inj NAHCO3 50 meq iv/ stat
9)temp monitoring 4th hourly
10) hourly abdomen girth monitoring
11) monitor vital (bp pr rr sp02
12) inj kcl 20meq iv/Stat






















Comments
Post a Comment