55Y Female with FEVER, SOB, PAIN ABDOMEN since 1 MONTH
- Get link
- X
- Other Apps
55Y Female with FEVER, SOB, PAIN ABDOMEN since 1 MONTH
July 12, 2023
Introduction: This is an online E-log Entry Blog to discuss, understand and review the clinical scenarios and data analysis of patients so as to develop my clinical competency in comprehending clinical cases, and providing evidence-based inputs.
CHIEF COMPLAINTS:
1. Fever since 1 month.
2. Dry cough since 1 month.
3. Shortness of breath since 1 month.
4. Pain abdomen since 1 month.
HISTORY OF PRESENTING ILLNESS:
- Patient was apparently asymptomatic 1 month back then she developed Fever. - Low grade, intermittent in nature, insidious in onset, gradually progressive, relieved on taking medication. - Fever increased from the past 4 days and is associated with generalized weakness, headache and body pains. - Not associated with chills and rigors.
- H/O Shortness of breath since 1 month, initially grade I which was insidious in onset, gradually progressed to grade III since 1 week. - No h/o orthopnea, PND.
- H/O dry cough associated with fever episode, increased since 1 week.
- H/O Pain abdomen since 1 month in the epigastric region on inspiration. - Insidious in onset, gradually progressive, non-radiating, no aggravating and relieving factors. - Associated with bloating and distention, nausea (more in the mornings), occasional vomiting episodes - nonbilious, nonprojectile.
- H/O pain in multiple small joints of hands, knee, shoulders in the last 10 years on and off and has used ayurvedic medicine for the same.
- Patient was found to have high BP recordings 5-6 months back and used oral medication on and off given by local practitioner.
- Patient is not a known case of Diabetes Mellitus, Thyroid disorders, Seizures, Tuberculosis, Asthma, stroke or any cardiac disorder.
- History of previous surgery - Cataract surgery for left eye 3 years back.
- Her appetite has decreased since past 1 week, she consumes a mixed diet.
- Sleep is adequate.
- Bowel movements decreased since 10 days (constipation) and Bladder movements are normal.
- No history of smoking.
- Occasional toddy drinker.
- No known food or drug allergies.
- Menstrual History: Attained menopause.
- No similar complaints in the family members.
GENERAL PHYSICAL EXAMINATION:
Examination has been done in a well-lit room in supine and sitting posture after taking informed consent and after reassuring the patient.
- Patient was conscious, coherent, co-operative and well oriented to time, place and person.
- Moderately built and nourished.
- Pallor present.
- No signs of Icterus, Cyanosis, Clubbing, Pedal edema, Generalized Lymphadenopathy.
- JVP normal.
11/07/2023
Temperature - 102.7F
Respiratory Rate - 30 cpm
Pulse Rate - 106 bpm
Blood Pressure - 140/90 mm Hg
SpO2 - 97 at room temp
GRBS - 140mg%
12/07/2023
Temperature - 98.6F (Fever spike +)
Respiratory Rate - 20 cpm
Pulse Rate - 98 bpm
Blood Pressure - 130/80 mm Hg
SpO2 - 97% at RA
GRBS - 194mg%
13/07/2023
Patient is conscious, coherent, cooperative.
Pain abdomen increased in intensity, patient not passed stool.
Temperature - 99.8F
Respiratory Rate - 26 cpm
Pulse Rate - 100 bpm
Blood Pressure - 130/70 mm Hg
SpO2 - 92% at RA; 99% at 2L o2
14/07/2023
Patient is conscious, coherent, cooperative.
Pain abdomen increased in intensity since last 3 days, associated with 3 episodes of bilious vomitings, non-projectile, non-blood stained, non-foul smelling.
Stools passed today (greenish in colour)
Temperature - 100F (Fever spike +)
Respiratory Rate - 30 cpm
Pulse Rate - 104 bpm
Blood Pressure - 130/80 mm Hg
SpO2 - 90% at RA, 98% at 2L o2
Central Nervous System: No abnormality detected.
Per Abdomen:
Distended
Guarding + in right hypochondrium
Tenderness in epigastrium and right hypochondrium +
Bowel sounds +
Hepatomegaly +
Cardiovascular System:
On Inspection: -
1. Precordium:
- No precordial bulges.
- No engorged veins.
- No scar/sinus.
- No epigastric pulsations
2. Chest wall Defects: None.
On Palpation:-
- Apical beat can be localized 1cm lateral to the midclavicular line in the 6th Intercostal Space.
- Palpable P2 +
- Parasternal Heave: Absent
On Percussion: -
Cardiac dullness
On Auscultation: -
- S1, S2 heard.
- No murmurs heard.
Respiratory System:
- Crepitations heard in B/L Basal lung areas (ISA and IAA).
- Bilateral air entry is present.
- Normal vesicular breath sounds are heard.
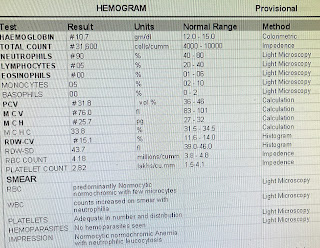
INVESTIGATIONS:
10th JULY
2. Blood Urea: 41 mg/dl (normal 12-42)
3. RBS: 121mg/dl
12th JULY
Blood Urea: 43mg/dl
PROVISIONAL DIAGNOSIS:
- Get link
- X
- Other Apps



.jpeg)