final practical examination short case
- Get link
- X
- Other Apps
General medicine E - LOG Book
Final practical examination : short case
Hall ticket no : 1701006198
This is an online E-log book to discuss our patient de-identified healthdata shared after taking his/ her guardians sign informed consent
Here we discuss our individual patient problems through series of inputs from available Global online community of experts with an aimto solve those patient clinical problem with collective current bestevidence based inputs.
This E-log also reflects my patient centered online learning portfolio. I have been given this case to solve in an attempt to understand thetopic of " Patient clinical data analysis" to develop my competancy inreading and comprehending clinical data including history, clinicalfinding, investigations and come up with a diagnosis and treatmentplan.
Case presentation :
22 Year old Male patient came to the opd with the chief complaints of
abdomen pain since 4 days
History of presenting Illness:
Patient was apparently asymptomatic
4 months back then he developed abdomen pain and vomiting
presenting to a hospital diagnosed as Acute Pancreatitis. He was
treated at the hospital and was discharged with the advice to stop
drinking alcohol.
Then 4 days back , he developed pain over upper abdomen which
is of dragging type, radiating to back aggravated on lying down.
Patient denies history of fever, nausea, vomiting and diarrhoea.
Patient also gives history of alcohol withdrawal symptoms after
the pancreatits episode 4 months back and desries to take up a
treatment for deaddiction
Past History:
Not a known case of Diabetes mellitus, Hypertension. Epilepsy,
Cardiovascular diseases. Asthma and tuberculosis
Family History: No similar complaints in family
Not significant
Personal history:
Takes mixed diet, has a reduced appetite
Sleep is Adequate
Bowel and bladder habits are regular
Addictions: Started drinking alcohol 4 years back with friends
and later the amount of alcohol incresed to 12 units. Started taking
alcohol daily since 3 years.
Reduced intake to 3 units since 3 months. Last intake
was 5 days back of about 6 units of alcohol.
Smokes 3-5 beedies per day
General physical examination: Patient is conscious, cooperative and
well oriented to time, place and person.He is of thin built.
No signs of pallor, icterus, cyanosis, clubbing. lymphadenopathy
edema present
Vitals:
Patient is afebrile
Pulse rate: 92 bpm
Blood pressure: 110/80 mm of Hg
Respirtaory rate: 14 cpm
Systemic Examination:
ABDOMEN EXAMINATION
INSPECTION:
Shape – Flat
Umbilicus –central in position
All quadrants of abdomen are moving equally with respiration.
No dilated veins, hernial orifices, sinuses
No visible pulsations.
PALPATION:
No local rise of temperature and tenderness
All inspectory findings are confirmed.
No guarding, rigidity
Deep palpation- no organomegaly.
PERCUSSION:
There is no fluid thrill , shifting dullness.
Percussion over abdomen- tympanic note heard.
AUSCULTATION:
Bowel sounds are heard.
Investigations:
Serum Lipase: 112 IU/L (13-60)
Serum Amylase: 255IU/L (25-140)
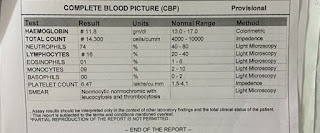
Hemogram:
Hemoglobin: 11.8 mg/dl
Total leucocytes: 14,300 cells/cumm
Lymphocytes: 16(18-20)
Provisional diagnosis: Pseudocyst of pancreas with unresolved acute pancreatitis .
Treatment:
Nill By Mouth
Intravenous fluids Ringer lactate and normal saline 10ml per hour
Inj. TRAMADOL 100 mg in 100ml normal saline IV BD
INJ. ZOFER 4mg IV BD
INJ. PAN 40 MG IV BD
INJ. OPTINEURIN 1amp in 100 ml nd IV OD
Psychiatric medication:
TAB. LORAZEPAM 2mg BD
TAB. BENFOTIAMINE 100mg OD
- Get link
- X
- Other Apps